Abstract
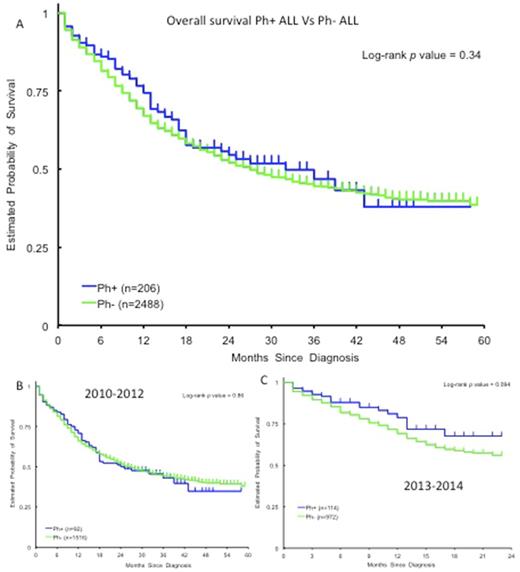
Translocation between chromosome 9 and 22 results in a BCR-ABL1 fusion gene identified in the form of an abnormal chromosome 22 (Philadelphia chromosome or Ph) in cytogenetics and/or other molecular studies. Ph+ acute lymphoblastic leukemia (ALL) constitutes about 25% of patients with pre-B ALL with increasing incidence with age. Prior to the introduction of tyrosine kinase inhibitors (TKI), presence of Ph chromosome conferred a poor prognosis in patients with ALL. Based on post-hoc comparisons between prospective clinical trials conducted before and after the introduction of this class of drugs, it appears that the use of TKIs inhibiting BCR-ABL have significantly improved the survival in Ph+ ALL. However, there has been no large-scale population based study comparing the survival of Ph+ ALL with Philadelphia negative (Ph-) ALL in the period when TKIs were widely used for treating Ph+ ALL. This information is highly relevant because survival of patients on clinical trials often exceeds results seen in real world. This could be due to study exclusion criteria, disparities in the number of elderly patients who receive TKI therapy, omission of patients with CNS involvement, etc. Thus the apparent improvement in outcomes has awaited confirmation at the population level. We compared the survival of Ph + and Ph-ALL during the period when TKIs were universally available in the US for Ph+ ALL, using a Surveillance, Epidemiology, and End Results (SEER) Database analysis. Patients with pre-B ALL ≥18 years in age, diagnosed between 2010 and 2014 were identified in SEER registries. 2694 patients with pre-B ALL were identified (206 Ph+ALL and 2488 Ph-ALL). The median OS was 32 months in Ph+ALL (95% CI 18 months-NE) and 27 months (95% CI 24-30 months) in Ph-ALL (Log-rank test p-value 0.34). To evaluate the progress in the survival of Ph+ ALL compared to Ph- ALL with time, the OS was estimated separately for patients diagnosed between 2010 - 2012 and 2013 - 2014 (Figure 3B and 3C). For 2010-2012, there was no significant difference (Log-rank p-value = 0.86) in the OS between Ph+ ALL (median OS = 24.5 months, 95% CI = 17.0-43.0) and Ph-ALL (median OS= 27, 95% CI = 23.0 - 30.0). For patients diagnosed between 2013 - 2014 period, there was a trend towards better survival for patients diagnosed with Ph+ ALL (1-year survival rate: 78.8%, 95% CI= 67.1%-86.7%) compared to Ph- (1-year survival rate: 69.2%, 95% CI= 65.5%-72.6%), although the difference was not statistically significant (Log-rank p-value = 0.094). Older age was associated with worse prognosis in both Ph+ALL and Ph-ALL. Age-adjusted OS was inferior in Hispanics and African-Americans compared to non-Hispanic whites. Survival of pre-B ALL shows continued improvement with time. Philadelphia chromosome status does not confer poor prognosis in pre-B ALL in the TKI era. Prognostic factors in pre-B ALL should be re-evaluated in the light of this finding.
Kelly: Amgen: Honoraria; Abbvie: Honoraria; Jannsen: Honoraria; Pharmacyclics: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal